Sleep and Cancer
Getting a restful night’s sleep is a challenge for many cancer patients. Pain from the cancer itself, fatigue and discomfort from chemotherapy, and medication side effects are just a few of the things that make sleep elusive for cancer patients. Worse, not getting enough sleep weakens the immune system and can exacerbate symptoms or negative side effects.
An increasing amount of research has found links between poor sleep and several cancers. Keep reading to learn what the latest research suggests about the connection between cancer and sleep, and how you can get better sleep if you’re undergoing cancer treatment.
Does lack of sleep cause cancer?
Regularly getting a good night’s sleep is an essential part of your overall health. While sleep itself has not been deemed a causal factor for cancers, researchers have associated certain sleep disorders with an increased risk of cancer. The three main sleep issues correlated with cancer are chronic sleep deprivation, sleep apnea, and shift work sleep disorder.
Sleep deprivation and cancer
Anyone who has missed a night’s sleep understands the reality of sleep deprivation. Lack of sleep worsens your mood, increases fatigue, and reduces your ability to concentrate. Chronic sleep deprivation (getting less than sufficient sleep over a sustained period of time, usually 7 to 8 hours for adults) is associated with:
- Poorer memory and cognitive processing skills
- Weakened immune system
- Weight loss or weight gain
- Increased irritability and higher risk for depression
- Poorer judgment
Individuals may experience sleep deprivation as a result of hectic work-life schedules, comorbid conditions such as depression or insomnia, or environmental factors like noisy bedroom environments.
Unfortunately, multiple studies have linked sleep deprivation with increased cancer risk.
- Men with insomnia were twice as likely to develop prostate cancer, according to a 2014 study that followed more than 2,000 men over a five-year timeframe.
- Individuals who averaged fewer than 6 hours of sleep per night (below the recommended amount of 7 to 8 hours) had a 50 percent increased risk of colorectal cancer, according to a 2010 study.
- Lack of sleep is correlated with more aggressive forms of breast cancer, according to a 2012 study of postmenopausal women. They found that breast cancer patients who regularly slept fewer hours of sleep tended to have more aggressive forms than women who slept longer.
Sleep apnea and cancer
Sleep apnea describes sleep-disordered breathing where the individual literally stops breathing for up to a few seconds during sleep. The resulting gasping, choking, or loud snoring may wake the person up multiple times throughout the night, so they experience disrupted sleep. Sleep apnea is typically caused by an obstruction of the airways.
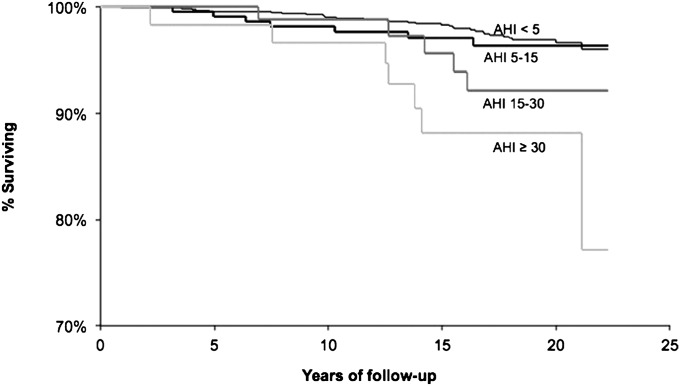
For some time, sleep apnea has been linked with obesity, diabetes, and cardiovascular disease. Recent research also suggests a link between sleep apnea and cancer. 80 percent of head and neck cancer patients also have sleep apnea. Spanish researchers found that individuals with severe sleep apnea had a 65 percent increased risk of cancer, and a Wisconsin-based study found individuals with the highest amount of apnea-hypopnea episodes were 5 times more likely to die from cancer than those without sleep apnea.
The chart below from the Wisconsin study shows the correlation between AHI and reduced cancer survival rate. AHI, short for Apnea-Hypopnea Index, measures the severity of an individual’s sleep apnea.
Animal studies replicate these findings. According to a 2014 study published in the journal Cancer Research, animal researchers linked the fragmented sleep from sleep apnea with accelerated cancer growth in mice. The researchers placed mice with tumors in low-oxygen environments (to mimic the effects of having sleep apnea), and their cancer progressed at an accelerated rate.
Researchers theorize that the oxygen deprivation associated with sleep apnea may be what’s causing the cancer. When the body doesn’t get enough oxygen, it grows more blood vessels as a way to compensate, which in turn enables cancer tumors and tissue to grow faster.
Shift work sleep disorder and cancer
Researchers have established a link between circadian rhythm disorders, in particular shift work sleep disorder, and increased risk of breast, colon, ovary, and prostate cancers.
Circadian rhythm disorders occur when an individual’s biological clock becomes out of synch with the external environment. Many of us have experienced jet lag, a circadian rhythm disorder that happens when you travel across time zones and your body hasn’t quite synchronized with the day-night cycle of your new location. Shift work sleep disorder affects shift workers, especially those on night shifts or rotating shifts, who are awake during times when the body expects you to be asleep. Common symptoms include insomnia, microsleep episodes, fatigue, and poorer mood and concentration.
Multiple studies have studied the effects of shift work on breast cancer risk. Women who worked night shifts for 4 years and those who worked fewer than 3 night shifts per week both had a 30 percent higher risk of breast cancer than women who did not perform shift work at all, according to a 2012 study published in the International Journal of Cancer. In the first group, the women had entrained their bodies to the opposite of the normal day-night cycle, having worked night shifts regularly for several years. The second group of women never got a chance to fully get used to one schedule over the other, daytime or night. Both scenarios increased their risk of breast cancer.
Even if shift workers get sufficient sleep, researchers suspect the issue may be the disruption to their “normal” circadian rhythms. During shift work, the body is exposed to light during times when it should be asleep. Besides regulating your sleep and wake cycle, your circadian clock directs a variety of biological functions, including organ function, hormone production, and body temperature. The impact to these other functions could also create a conducive environment for cancer to grow.
Most critically, though, disrupting your circadian clock can delay melatonin production (the hormone responsible for sleep) and impact the body’s overall levels of melatonin. When scientists alter the sleep wake cycles of rodents in the lab, cancer also grows at an increased rate. Researchers suspect these decreased melatonin levels may facilitate cancer growth.
For example, a 2003 Boston study found reduced melatonin levels were associated with an increased risk of breast cancer. Here, the researchers think the issue lies with the increased estrogen production, which occurs when melatonin levels are lower. Increased estrogen production is yet another risk factor for breast cancer.
Further cementing the link between melatonin levels and cancer, a Michigan State University study found that treating breast cancer stem cells with melatonin reduced the number and size of breast cancer tumors, suggesting that the antioxidant properties of melatonin could eventually be used as a treatment for stopping the growth of breast cancer tumors.
The increased cancer risk for shift workers may also have something to do with their cortisol levels. Cortisol production operates in inverse to melatonin – cortisol levels peak in the morning after sleep and decline during the day. Female night shift workers have a “shifted cortisol rhythm” and peak in the afternoon instead of at dawn when they’re supposed to.
How does cancer affect sleep?
Between 30 to 75 percent of people receiving cancer treatment have some sleep problems and about 25 percent of cancer survivors continue to have issues sleeping. Lung cancer patients tend to report the most sleep problems.
The side effects of cancer and treatment cause a host of issues that can make falling and staying asleep more difficult. Individuals with cancer may have increased anxiety and depression, two conditions that go hand-in-hand with insomnia. Extensive treatment can cause excessive fatigue and cancer-related sleep disorders. Hot flashes and night sweats are common side effects that make it challenging to get comfortable enough to fall asleep.
Generally, the three largest sleep issues affecting cancer patients are insomnia, excessive daytime sleepiness, and restless legs syndrome.
Insomnia
While insomnia isn’t typically a common side effect of the chemotherapy itself, many of the associated medication, especially steroids, can cause disrupted sleep. Worse, insomnia often exacerbates other symptoms and side effects from the cancer treatment. Some estimates report insomnia affecting one-third to one-half of cancer patients, which is two to three times higher than the general population.
Insomnia describes a general difficulty falling or staying asleep on a regular basis. Among cancer patients, the most commonly reported symptoms of insomnia include:
- Frequent nighttime awakenings (76%)
- Difficulty falling asleep (44%)
- Waking up too early (33%)
Chemotherapy drugs can cause fatigue, so patients are more prone to nap during the day, leading to insomnia at night. The drugs used to manage the side effects of chemotherapy can also cause sleep problems: anti-nausea medications may cause drowsiness, while the energizing nature of steroids make it difficult to fall asleep.
Combine all this with the emotional distress of having cancer, and the anxiety and worry which may keep one up at night.
Excessive daytime sleepiness and fatigue
Excessive daytime sleepiness and fatigue are highly correlated with insomnia. In one study of cancer patients, those who reported fatigue were 2.5 times more likely to also have insomnia.
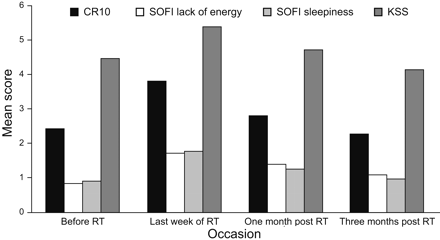
While fatigue and excessive daytime sleepiness are clinically distinct, they can feel similar to the individual living with them. Fatigue refers to a feeling of low energy and exhaustion, which often causes the individual to seek napping as a way of relief. As alluded to above, fatigue is a common side effect of cancer treatment. Individuals undergoing radiotherapy reported nearly double the amount of fatigue after receiving radiotherapy than before treatment. Fortunately, the fatigue returned to normal levels after a period of months.
As antiemetic medications are prescribed to reduce symptoms of chemotherapy-induced nausea and vomiting, they may introduce new sleep-related symptoms of their own, like excessive daytime sleepiness (EDS). EDS describes a sense of drowsiness that lingers throughout the day, even after adequate sleep. While EDS is different than fatigue, sufferers seek relief in similar ways: napping. If the individual naps for too long, it makes it much harder for them to fall asleep at night, creating a negative cycle of insomnia.
Restless legs syndrome
Cancer patients undergoing chemotherapy may experience disturbed sleep due to restless legs syndrome. Restless legs syndrome (RLS) is characterized by a strong urge to move the lower limbs in order to relieve a “pins and needles” sensation that develops when the individual is in a supine position.
The constant need to move their legs to find relief disrupts the individual’s ability to fall asleep in the first place, as well as their ability to stay comfortably asleep.
RLS may affect between 5% to 10% of people. Some studies have found cancer patients are twice as likely to have RLS, especially women with breast cancer and men 50 and older who have prostate cancer.
RLS also shares a direct relationship with increased levels of anxiety and depression, and lower quality-of-life scores among cancer patients. In turn, both anxiety and depression are highly correlated with insomnia.
Tips for getting better sleep when you have cancer
Getting sufficient sleep on a consistent basis improves your mood and your cognitive functioning, and it keeps your immune system strong. If you have cancer or care for someone who does, some of the following therapies or products may help you get more quality sleep.
Therapeutic approaches to better sleep for cancer patients
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) has proven helpful for cancer patients who suffer from insomnia.
CBT involves techniques that help the patient reframe their emotions and thoughts around sleep. Patients learn relaxation techniques and deep breathing exercise to quiet racing thoughts and help them fall asleep. They may also practice stimulus control techniques, which limit the time spent in bed and retrain the mind to see the bed as only for sleep. Progressive muscle relaxation involves tensing and relaxing the muscles in an ordered fashion that promotes restfulness.
Sleep restriction therapy
Sleep restriction therapy is another behavioral technique used to addressed insomnia. Individuals decide on a set sleep and wake schedule, and adhere to that no matter what. They don’t take naps during the day, and are only allowed to spend the allocated time in bed, regardless of whether they sleep the whole time. Ideally, eventually their daytime fatigue disappears and the individual trains their body to sleep during the scheduled time frame.
Light therapy

Source: Reader’s Digest
Light therapy employs light boxes, tables, or specialized lamps to help individuals who have an offset circadian clock, whether due to shift work, jet lag, or blindness. The individual sits in front of the light device for a set amount of time in the morning or afternoon, depending on how their circadian cycle is offset. A current clinical trial is testing the effectiveness of light therapy eyeglasses to help lung cancer patients who suffer from insomnia and fatigue.
Sleep products for cancer patients
Cooling mattresses
Cancer patients who experience night sweats or postmenopausal breast cancer patients with hot flashes often have difficulty staying asleep due to overheating. Mattresses with superior temperature regulation, such as innerspring mattresses and airbeds, stay cooler than memory foam mattresses that envelop the body.
Cooling pillows
Patients can also purchase cooling pillows for the home and to take with them to chemotherapy appointments. These pillows are made with more breathable materials—like moisture-wicking wool and gel-infused foam—which are designed to stay cool all night.
White noise machines
White noise machines, available as standalone devices or as smartphone apps, play static white noise, nature sounds, or calming melodies designed to soothe one to sleep. They’re often used by individuals with insomnia. There are even travel-size versions to take with you to chemotherapy. Just make sure you pick a different white noise playlist that you can associate with relaxation, as opposed to sleep. You don’t want to accidentally induce a midday nap.
Anti-snoring products

Source: Wikipedia
There are many anti-snoring products that help keep the airways open and enable the sleeper to breathe properly throughout the night. Anti-snoring mouthpieces fit between the teeth to reduce symptoms, and nasal vents fit in the nostrils. For individuals with extreme sleep apnea, continuous positive air pressures (CPAP) machines are recommended.
CBD oil
CBD oil has been shown to provide various benefits for cancer patients, from pain relief to sleep. It’s also proven to be more effective than traditional medication in relieving chemotherapy-related nausea and vomiting Not to be confused with THC, CBD oil is a 100% non-psychoactive hemp extract that’s legal throughout the United States. CBD oils are available in a variety of product types, including oil tinctures, softgel capsules, gummies, and topical products.
Weighted blankets
Individuals with restless legs syndrome often find weighted blankets help reduce symptoms. Experts recommended getting a blanket that weighs 10 percent of your total body weight plus 1 pound.
Behavioral approaches to better sleep
Avoid naps
Naps are very tempting to anyone experiencing fatigue or daytime sleepiness, but they only reinforce insomnia. If possible, do your best to avoid napping during the day. If you absolutely need to nap for relief, limit your nap to 20 minutes at the most. This is short enough to keep you in light sleep, so it won’t disrupt your sleep cycle later that evening.
Practice good sleep hygiene
Good sleep hygiene involves going to bed and waking up at around the same time every day, reserving the bedroom for sleep and sex only, and avoiding heavy meals, caffeine, alcohol, and intense exercise in the hours leading up to bedtime.
Keep the bedroom cool and dark
A cool, dark bedroom is the optimal environment for sleep. Set up blackout curtains or wear an eye mask to block out ambient light at night, and turn the temperature down to somewhere in the mid-60 degrees Fahrenheit. That’s the recommended temperature for sleep, but if you’re experiencing night sweats, you may want to lower it even more.
Follow a bedtime routine
In addition to following a regular sleep schedule, you can further train your mind to prepare for sleep by establishing a pre-bed ritual. Engage in the same set of activities every night before bed. The activities should be calming, like meditation, aromatherapy, or a warm bath.
Additional resources
For better sleep:
- Understand more about the unique sleep issues affecting shift workers, and treatment options and resources for individuals with shift work sleep disorder.
- Learn more about how light therapy helps circadian disorders, and how you can get started.
- Read more about cognitive behavioral therapy techniques and how it helps insomnia.
- There are many products designed for helping individuals with disabilities get better sleep. Many of these products may also be helpful for addressing the pain and sleep issues associated with cancer treatment.
For all cancers:
- The American Cancer Society offers a 24-hour helpline (800-227-2345) and Live Chat, as well as online support communities, local support groups, volunteer events, and research.
- The National Cancer Institute is part of the National Institutes of Health. As the largest funder of cancer research globally, NCI publishes research and shares training for doctors and health professionals
- Founded by testicular cancer survivor Lance Armstrong, the Livestrong Foundation provides online resources and community support programs, as well as one-one-one personalized care plans and support for patients and caregivers.
- The Cancer subreddit connects cancer patients, survivors, and loved ones with each other to share stories, news, and support. There are also many subreddits devoted to specific forms of cancer.
- The Cancer Forums claim over 50,000 members of cancer patients and survivors, loved ones, and caregivers. The site hosts over 20 forums dedicated to specific types of cancer.
For breast cancer:
- Well known for making the pink ribbon symbol ubiquitous, the Susan G. Komen Breast Cancer Foundation is the largest breast cancer organization in the United States. They host Race for the Cure fundraising events and offer a helpline available during weekday hours ((877-465-6636).
- The BreastCancer.org Community is an online forum of nearly 200,000 members, including current patients, caregivers, survivors, and family members affected by breast cancer.
For prostate cancer:
- The Prostate Cancer Foundation is the largest organization focused on funding prostate cancer research and connecting patients with treatment centers and clinical trials.
- ZERO works to provide education, financial assistance, and free case management to men diagnosed with prostate cancer. The organization also hosts fundraising walk/run events.
