Women and Insomnia
Women are more prone to insomnia than men. More women have frequent bouts of sleeplessness (several times a week) than men, and this tendency extends over all periods of life. Not only that, but as people age, the gap between women and men increases. Women under 45 years old have an incidence 1.4 times that of men of the same age. Among older populations, women are 1.7 times more likely to have insomnia.
Women are almost twice as likely to use sleep aids than men, according to the CDC.
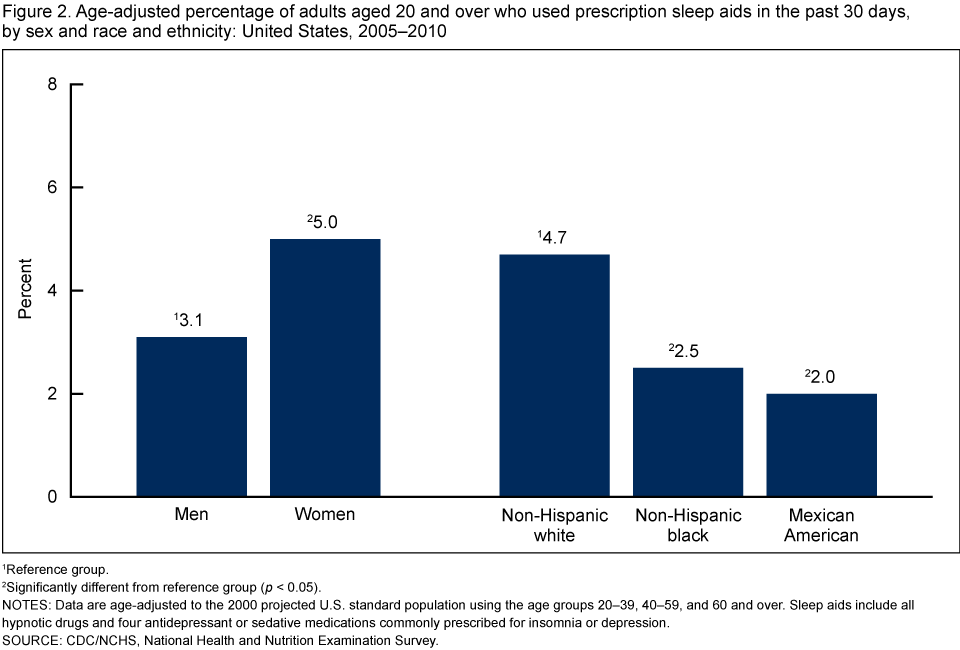
Source: CDC
Do hormones cause insomnia? Many women experience insomnia when they have fluctuations in the serum levels of hormones. These times include during their monthly cycle, pregnancy, and menopause.
How does menopause affect your sleep?
Menopausal insomnia can begin with perimenopause – the stage before menopause women experience in their late 30s or 40s. On average, perimenopause lasts about 4 years, and ends when a woman hasn’t had her period for at least 12 months.
Perimenopause and menopause cause hormonal changes, at the same time when women are often undergoing other major lifestyle changes such as retirement and empty nesting. During perimenopause, women’s ovaries begin decreasing hormone production of estrogen and progesterone. Progesterone helps to promote sleep while estrogen affects emotional well-being. Decreased levels of these hormones can make it more challenging to emotionally deal with the stressors of the body changes of menopause, in addition to the lifestyle changes that occur at the same time.
20% of women experience depression during menopause, whether brought on by the loss of estrogen, the lifestyle changes that often accompany menopause, or a combination of the two. Depression is often a comorbid condition of insomnia, as are stress and anxiety.
Menopause causes other bodily changes, most notably hot flashes. 75% of women experience hot flashes during menopause. Hot flashes result in elevated body temperature and night sweats, both of which make it tougher to fall asleep and stay asleep. The energizing heat from a hot flash awakens the mind as well. Cool temperatures are conducive to sleep, and the body naturally cools down before bedtime as part of the circadian rhythm. Hot flashes, especially ones that contribute to night sweats, interfere with the body’s ability to cool down and stay asleep.
As women transition into menopause in their 40s to 50s, other physical changes occur naturally, thanks to the aging process. Older adults may wake more frequently during the night, due to incontinence and reduced bladder control. Adults also spend less time in restorative REM sleep as they age and rise earlier, which can result in daytime sleepiness and insomnia.
Tips for managing menopausal insomnia
Anyone with insomnia may find relief by following a regular sleep schedule and practicing good sleep hygiene. However, menopausal women suffering from hot flashes and night sweats may find the following additional tips helpful.
1. Lower the bedroom temperature
A cool temperature in the mid-60 degrees Fahrenheit is ideal for sleep, but menopausal women may want to take it a few degrees cooler.
2. Keep cool reinforcements by the bed
Have a cool glass of water, an extra pillow or pillowcase, and an extra set of breathable pajamas near the bed, so you can easily change or cool down during the night from night sweats. You may keep a washcloth in a bucket of ice nearby as well.
3. Invest in a mattress with excellent temperature regulation
Certain mattresses trap heat more than others and can intensify the effects of hot flashes. The best mattresses for hot sleepers are firm innerspring mattresses or airbeds.
4. Try meditation, acupuncture, and relaxation exercises
Acupuncture has been shown to help relieve insomnia. Breathing exercises and meditation techniques can also help quiet the mind before bed.
5. Manage diet and exercise
Avoid alcohol and stimulants like caffeine, especially before bed. These interfere with sleep onset generally, but can also trigger hot flashes for peri- and postmenopausal women. Eat dinner two to four hours before bed, and exercise earlier in the day if possible (to avoid elevating your body temperature before bed). Exercise improves mood and exhausts the body, making it easier to fall asleep at night.
6. Use a white noise machine or smartphone app
Many people use white noise as a sleep aid to quiet the mind and induce a restful state. White noise machines are widely available, as are smartphone apps with white noise or nature sound libraries.
7. Ask your doctor about other treatment options
For moderate to severe hot flashes that interfere with sleep, some doctors may recommend hormone replacement therapy (HRT) or prescribe low-dose antidepressants like Prozac and Paxil. However, HRT is currently only recommended as a temporary solution, given its connection with increased risk for breast cancer, blood clots, heart disease, and stroke. Some perimenopausal women have found combination birth control pills effective for relieving insomnia symptoms.
Can your period give you insomnia?
Premenstrual syndrome (PMS) seems to cause both insomnia and hypersomnia. Different women experience different symptoms. Many menstrual symptoms like bloating and cramps cause physical discomfort that make it tougher to sleep. Emotional variability, irritability, stress, and fatigue can also can contribute to insomnia.
In the first half of the menstrual cycle (the follicular phase), the body increases estrogen production leading up to ovulation. After ovulation, in the second half of the cycle (the luteal phase), progesterone production rises and has a soporific effect. In the days before the period begins, both hormones levels drop which can cause insomnia.
Source: BBC
Women experience less REM sleep in the luteal phase of their cycle, which may help explain insomnia during PMS, according to a 2010 study. During this stage, the increased progesterone production after ovulation increases the core body temperature by up to half a degree. Since REM sleep corresponds with the lowest body temperatures during the night, this may explain why REM sleep is tougher to achieve during the second half of the menstrual cycle.
Tips for managing PMS insomnia
Women with insomnia may find relief by following a regular sleep schedule and practicing good sleep hygiene.
1. Keep the bedroom cool and dark
A cool temperature in the mid-60 degrees Fahrenheit is ideal for sleep. Stop using electronics at least an hour before bed and avoid blue light.
2. Try meditation, acupuncture, and relaxation exercises
Acupuncture has been shown to help relieve insomnia. Breathing exercises and meditation techniques can also help quiet the mind before bed.
3. Manage diet and exercise
Avoid alcohol and stimulants like caffeine, especially before bed. Eat dinner two to four hours before bed, and exercise earlier in the day if possible (to avoid elevating your body temperature before bed). Exercise improves mood and exhausts the body, making it easier to fall asleep at night.
4. Use a white noise machine or smartphone app
Many people use white noise as a sleep aid to quiet the mind and induce a restful state. White noise machines are widely available, as are smartphone apps with white noise or nature sound libraries.
5. Ask your doctor about other treatment options
Sleep restriction has been found to reduce menses-related depression, as has bright light therapy for insomnia. Premenstrual dysphoric disorder (PMDD) also is associated with sleep disruption, although doctors more commonly address the anxiety symptoms than insomnia. Some doctors may prescribe antidepressants or Z-drugs for PMDD and PMS, which may help address related sleep problems.
Insomnia during pregnancy
Pregnancy-induced insomnia can often be caused by physical discomfort, especially during the first trimester, when the body is first introduced to all the physical, mental and emotional changes associated with pregnancy, and the third trimester, by which point over 75 percent of pregnant women report experiencing insomnia. Hormonal changes, reduced bladder capacity, pregnancy-related heartburn, leg cramps, and nerves about labor all contribute to insomnia for expectant mothers.
Tips for managing pregnancy-related insomnia
Women with insomnia may find relief by following a regular sleep schedule and practicing good sleep hygiene. However, pregnant mothers may find the following additional tips helpful.
1. Keep the bedroom cool and dark
A cool temperature in the mid-60 degrees Fahrenheit is ideal for sleep. Stop using electronics at least an hour before bed and avoid blue light.
2. Invest in maternity pillows
Reduce the physical discomfort caused by pregnancy by stocking up on multiple pillows. Sleep on your left side with a pillow at your back, with pillows to support both your arms and your legs.
3. Try meditation, stretching, and relaxation exercises
Breathing exercises and meditation techniques can help quiet the mind before bed. Stretching and prenatal massage can also reduce discomfort so it’s easier to get comfortable and fall asleep.
4. Manage diet and exercise
Minimize the stress on your bladder by reducing the liquid you drink at night. Avoid alcohol and stimulants like caffeine, especially before bed. Eat dinner two to four hours before bed, and exercise earlier in the day if possible (to avoid elevating your body temperature before bed). Exercise improves mood and exhausts the body, making it easier to fall asleep at night.
5. Use a white noise machine or smartphone app
Many people use white noise as a sleep aid to quiet the mind and induce a restful state. White noise machines are widely available, as are smartphone apps with white noise or nature sound libraries.
Other sleep disorders in women
In general, sleep disorders are more common in women than in men, and they play out differently, emerging throughout the reproductive life cycle. Although men are more likely to have obstructive sleep apnea than women, postmenopausal women are twice as likely to have OSA than premenopausal women.
Sleepiness leads to weight gain by discouraging physical activity. Depression leads to overeating. Social expectations of women may contribute to the greater prevalence of sleep disorders. They are more likely to be the primary caregiver than men and more likely to shoulder a larger share of the housework. Researchers have also found that on average women get 5% less deep sleep on average than men.
Women are more likely to have restless legs syndrome (RLS), and it’s even more common during pregnancy (by 26%). Researchers speculate RLS could be caused by an iron deficiency, which would explain why women with heavier periods are more likely to have RLS.
Women are also more likely to have depression, anxiety, and fibromyalgia all of which can contribute to insomnia.
